
Studerandebloggen/ Student blog
The Social Determinants of Health – Health Equity and Inequity

Authors:
Cecilia Mansén, BSc student, Bachelor in HealthCare, Nursing Novia UAS
Anita Wikberg, Supervisor, RN, RM, PhD, Senior Lecturer, Novia UAS
Abstract
We are far from a world where all can reach their full health potential despite any social disadvantages. To reach health equity, the social determinants must be addressed. These determinants include economic stability, access to quality education and health care, social and community resources and neighborhood context. Especially rural areas have limited capacity in implementing programs addressing these determinants. People with higher socioeconomic status live longer and healthier than those with poorer status. Social inequalities lead to health inequity. Policies are required to reach a more fear distribution of resources in society.
Introduction
Can all individuals achieve health? There exist several definitions of health. The first one of the three most used definitions being that health is when no disease or impairment is present. Together with the first, the second definition of health is when an individual can cope with the demands of daily life. The third definition views health as balance, when the individual is in harmony within and with the surrounding environment (Sartorius, 2006). The goal is when all individuals can achieve their full health potential despite any levels of underlying social disadvantages. This defines health equity and addressing the social determinants of health, is a step in the right direction to reach equity in health (Centers for Disease Control and Prevention, 2019).
What are the Social Determinants of Health?
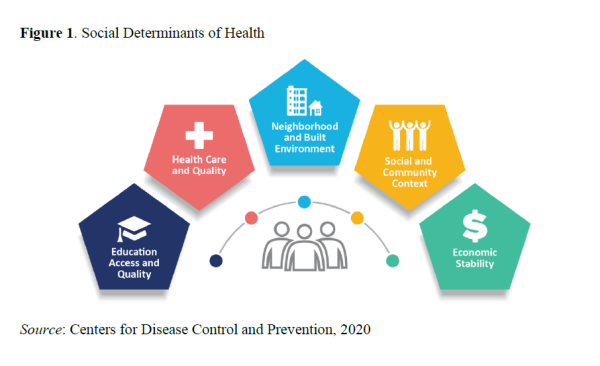
The world is constantly changing in the processes of globalization and modernization, especially in terms of global markets and economies. Countries with low- and middle-income are more affected by fluctuations in economy and growing inequalities. Economic growth in a country can improve average population health, meanwhile it can also widen the gap between the most and least advantaged people (World Health Organization, WHO, 2010). There are certain conditions persons are born into, grow up with and form social bonds, go to school, have careers and age. These conditions, or determinants, have an impact on health and quality-of-life outcomes. Social determinants of health are non-medical factors that affect individual health. As seen in Figure 1, these factors include socioeconomic status, education, residential location, living conditions, employment and access to health care. Differences in health occur in communities with low social determinants of health, for instance low personal income, living in poor and unsafe neighbourhoods and having inadequate education (Brown & Elliot, 2021).
Education Access and Quality
Access to education is one important social determinant of health. People who get quality education tend to stay in better health than those who do not. Education does not only put one in a better chance of future employment and therefor economic stability but is also a way of staying informed on how to take care of one's own health. It is not only about access to education, the programme and school a person is attending, should have health resources and supporting teachers to foster physical and mental development. Studies show that individuals with higher levels of education live longer and healthier lives. Adults who participated in quality education from childhood, were at lower risk for high blood pressure, obesity, elevated blood sugar and high cholesterol. The link between education and health is clear, the better the education, the greater chances for financial stability, which in turn allows for increased access to health insurance, quality food and sufficient housing in an unpolluted area. (Tulane University, 2021)
Quality Health Care
A crucial part of staying healthy means having access to quality health care and preventative services. One barrier to accessing health care is not having a health insurance, these individuals are less likely to have a primary health care provider or even afford treatment and medications. Other barriers include lack of availability, high cost and limited language access. These barriers prevent people from intervening in their own health and well-being. A reluctance to seek healthcare can mainly be seen in those with lower socioeconomic status. These individuals are less likely to be screened for chronic conditions such as cardiovascular diseases, asthma and certain cancers. (Singu et.al, 2020)
Health literacy can be described as the level to which a person can obtain, process and understand information regarding health and make appropriate health decisions. Culturally competent health care providers are needed to navigate and help individuals understand the situation and the healthcare system in order to make informed choices about their own health and well-being. A low health literacy correlates with a lower health outcome, not being able to understand health information and prescriptions makes it more difficult to take care of one’s own health. In other words, understanding various health risks and precautions needed, can reduce those risks and better take care of oneself (Health resources & Services Administration,2019). Health care professionals need to be aware of health illiteracy, it is common and reaches though all socioeconomic levels of society. There are strategies to improve health literacy. In a healthcare clinic the health care professional should use plain language with familiar words and short sentences. Another way of communication is through using images when informing about complex subjects. The health care professional can ask open-ended questions to determine the patient’s level of understanding. An effective method is the Teach-Back, meaning patients get to restate instructions and information given by the health care professional (Nierengarten, 2018).
Neighbourhood and Built Environment
There exist many people in the world living in neighbourhoods with high rates of violence, unsafe air and water access, pollution and other health and safety risks. Individuals with low income and ethnic minorities are more likely to live in areas with these health risks. Furthermore, some people working in unsafe environments, such as places with loud noises and smoke inhalation, are also exposed to health risks. These environmental contaminants can cause respiratory problems, nausea, fatigue and poisoning (Office of Disease Prevention and Health Promotion, 2021). The neighbourhood we live in have implications for our health but also the opportunity to be healthy. Health disparities can be studied by looking at different geographic locations. High poverty neighbourhoods are more likely close to factories and landfills that pollute the air and water with hazard particles. These areas often have higher rates of crime, are overcrowded and have minimal green space for physical activity. Families with low income, tend to live in poorer quality housing with infestation risks of mice and rats, lack of air-conditioning and mold. A study shows that 22% of children living in public housing were diagnosed with asthma compared to 7% of those children living in single family homes (Singu et.al, 2020).
Social and Community Context
Relationships and interactions between family, friends, co-workers and community members have an impact on an individual’s health and well-being. Making social connections and participating in community activities creates a feeling of belonging, which has shown to help manage mental health issues such as depression (Tulane University, 2021). Social capital is an indication of the shared resources within a community and the level of fairness, helpfulness and social trust it attains. An increase in income inequality decreases the social capital. Social capital can be seen as an element that links inequality and mortality. Civic activities and social cohesion are associated with lower neighbourhood violence and less stress and anxiety. Participating in civic activities, such as voting and volunteering, can make individuals stay more physically active and find a sense of purpose (Singu et.al, 2020).
Discrimination is socially structured and can intentionally or unintentionally cause harm to individuals and groups. Structural discrimination limit opportunities and resources of less privileged groups in society. Negative interaction on an individual level, such as between a healthcare worker and a patient based on for example ethnicity, religion or gender, is referred to as individual discrimination. This can negatively affect individuals and communities. Residential segregation is one example of structural discrimination that causes differences in health status because it determines the social and economic resources for individuals and communities. Regularly being discriminated is seen as a chronic stressor that increases susceptibility to physical illness and cause the body to be more physically sensitive in stressful social situations. (Office of Disease Prevention and Health Promotion, 2021)
Economic Stability
Financial health includes an economic ability to meet the basic needs of daily life and to have a financial freedom to make choices allowing one to enjoy life. Economic hardship is known to have a detrimental impact on a person's health and well-being. Economic stability means having energy security, housing security and food security, in other words having enough money to pay for electricity, heat, sufficient housing and enough quality food (Weida et.al, 2020). The issues related to economic instability not only affect people that live below the poverty line. The economic status directly affects the quality and quantity of food a person can purchase, the ability to prioritize physical activity and afford clothing and utensils needed in daily life and the ability to pay for medical care. An unstable housing situation causes plenty of stress in a person's life, moreover, not being able to afford enough nutritious food is associated with chronic diseases and, for a child it can mean malnutrition and developmental issues (North Carolina Alliance For Health, 2021).
Examples from Finland
A principal in Finland is that education is equal and free. However, a recent study (Laukkonen 2018) show that adolescents from low-income families are less likely to apply for universities. An explanation is that these students cannot afford preparation courses, unlike families with middle or higher income. A study conducted in Finland show that socioeconomic variables and health behaviours affect employment. Working before turning 18 years old is not abnormal, in year 2000, 17 percent of 9th graders were working beside school. Early employment can be negative, lower quality of life and heavy drinking are risks that have been reported. A poor socioeconomic background can lead to earlier employment also as a mean to fund higher education. Smoking and drinking affect health in adolescents and require spending more money, which in turn lead to even harder economic situation. The first paid employment is usually of low occupational class with adverse exposures of heavy physical workload, shift work and unforeseen contracts, which can have effects on future health. (Halonen et.al, 2019)
North Karelia is situated alongside the boarder to Russia and has been exposed to serious economic and political instability throughout the previous century. Over 400 000 Finns were forced to relocate in the 1940s due to Soviet annexation, leading to a rise in farming and particularly animal husbandry in the North Karelia region. In the 1960s, the area had the highest incidence of coronary heart disease mortality in Finland. Medical communities in Finland focused on behaviour modification, excluding structural changes and failing to address the social determinants of health. Fatty foods and dairy were cheap and part of culture, why buy special items from the store when there is milk and meat on the farm next door? East Finland Berry and Vegetable Project (1986) was an approach to increase fruit and vegetable consumption across the nation, trying to transition farmers from dairy products to berries. Instituted earlier, this project could have motivated people to change their food choices, without feeling they would hurt their or their neighbours’ livelihood. (Semler, 2021)
It is impossible to know the exact number of undocumented immigrants in Finland, although it is estimated to be 3000 to 10000 people. All undocumented immigrants have their own story, but they all have one thing in common, the uncertainty in not knowing what is next. Especially undocumented children are vulnerable, they are allowed in school but because they lack identification papers in Finland, they are at risk for social exclusion (Räsänen, 2020). For undocumented, only urgent healthcare are provided by the municipalities, they are also expected to pay the urgent care in full. However, municipalities can decide to grant illegal residents access to further healthcare. This is the case in Vantaa, where the municipality decided to grant undocumented pregnant women and children below 18 years, the same access to health care as any Finnish resident. Although the uncertainty for undocumented residents remain and most do not have access to health care (Savonius, 2017).
Challenges when Addressing Social Determinants
Compared to non-rural areas, people living in the rural counterparts have higher unemployment rate, lower educational systems and less access to social services and healthcare, factors that directly affect health and well-being. Rural communities more often experience limited availability and capacity to implement programs addressing the social determinants of health. Another limit is that rural areas more often struggle with getting the funding needed for these programs. Resource challenges also include shortage of staff. In USA, a fifth of the population live in rural areas where physician to patient ratio is 1 to 2500. There is a strong belief that health choices are made independently and with self-determination. This is an assumption that does not consider the social, cultural and environmental factors that contribute to health outcomes. Rural residents can experience stigma and social pressures when seeking help from certain health services. Cultural views and assumptions need to be considered when developing programs and services that focus on the social determinants of health. (Rural Health Information Hub, 2020)
Reaching for Health Equity
People with higher socioeconomic status have more opportunities to live prosperous lives and enjoy better health. The Commission on Social Determinants of Health has a vision, a world where all people have the chance to lead lives, they have reason to value. The aim of the commission is to encourage countries, global institutions and international organizations to improve population health and the distribution of health and ultimately reduce disadvantage due to ill health. Social inequalities cause inequities in health. Three principals have been proposed by the commission to tackle inequities in health: improving the conditions of daily life, work on the inequitable distribution of power, money and resources and lastly to measure the problem and evaluate action to raise public awareness about the social determinants of health. (World Health Organization, 2012)
Deliberate policy decisions are required to reach a fair distribution of benefits, guarantee food security, job security or access to affordable medication. Equity and its concepts must be understood and accepted among political and civil leaders for programmes to have an impact. Several factors, including politics, bureaucracy and civil society, are interfered when talking about change regarding social determinants. This requires leadership in order to mobilize and link interests together. Public health programmes must broaden to embrace a larger social, economic and developmental agenda, this means focusing on reducing health problems from the source. Improvements can be conducted regarding information systems to give better insight into specific determinants in the distribution of health in populations. Different interventions and packages shall be developed and tested. All public health programmes need to include an approach for the social determinants. Health programmes possess a responsibility to identify where interventions are possible, to propose a framework for monitoring the situation and to provide evidence of the relationship between socioeconomic factors and health. (WHO, 2010, p.264 - 280)
Conclusion
While a large part of the world is living longer and healthier lives, many are still being left behind with poorer health due to social determinants. There are several social determinants that can affect an individual's health. Imagine living in a rural area in a house with mold issues or working hard only to make minimum wages or attending a school that are short staffed in an area with high crime rates. The better education, the better chances of future economic stability through sufficient employment, which in turn increases the chances of living in better neighbourhoods and having better access to health care and health insurance. Actions must be taken to make sure the possibility for health is for everyone, reducing the existing health inequities. Through shared values, leadership, research, collaboration and awareness can policy decisions be made to act on the social determinants of health and reach for health equity.
References
- Brown, J. S., & Elliott, R. W. (2021). Social Determinants of Health: Understanding the Basics and Their Impact on Chronic Kidney Disease. Nephrology Nursing Journal : Journal of the American Nephrology Nurses’ Association, 48(2), 131–145.
- Centers for Disease Control and Prevention. (2019). NCHHSTP Social Determinants of Health. https://www.cdc.gov/nchhstp/socialdeterminants/faq.html?fbclid=IwAR0U4rHjUa2uCaIImKIW-EW8tJP1lau2IGKhAlPHlXlVZbQdbnHG4tF9KbY
- Halonen, J. I., Virtanen, M., Ala-Mursula, L., Miettunen, J., Vaaramo, E., Karppinen, J., Kouvonen, A., & Lallukka, T. (2019). Socioeconomic and health-related childhood and adolescence predictors of entry into paid employment. European Journal of Public Health, 29(3), 555–561. https://doi-org.ezproxy.novia.fi/10.1093/eurpub/cky221
- Health resources & Services Administration, HRSA. (2019). Health Literacy. Retrieved 9/2021 from https://www.hrsa.gov/about/organization/bureaus/ohe/health-literacy/index.html
- Laukkonen, M-L. (2018). Pienituloisten perheiden ylioppilaat va¨ltta¨va¨t riskia¨ pa¨a¨sykokeita painottavissa opiskelijavalinnoissa [High school graduates from low income families evade risk related to student admission emphasizing entrance examinations]. ETLA Brief 2018; No 62. Available at: http://pub.etla.fi/ETLA-Muistio-Brief-62.pdf.
- NIERENGARTEN, M. B. (2018). Improving health literacy: Ob/gyns can take simple steps to help patients understand their personal health information, promoting better outcomes. Contemporary OB/GYN, 63(6), 42–45.
- North Carolina Alliance For Health. (2021). Economic Stability: A Social Determinant of Health Category.https://www.ncallianceforhealth.org/economic-stability-a-social-determinant-of-health-category/
- Office of Disease Prevention and Health Promotion, ODPHP. (2021). Discrimination. Retrieved 9/2021 from https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/discrimination
- Office of Disease Prevention and Health Promotion, ODPHP. (2021). Neighborhood and built Environment. Retrieved 9/2021 from https://health.gov/healthypeople/objectives-and-data/browse-objectives/neighborhood-and-built-environment
- Rural Health Information Hub, RHIHub. (2020). Challenges and Barriers to Adressing Social Determinants of Health in Rural Areas. Retrieved 9/2021 from https://www.ruralhealthinfo.org/toolkits/sdoh/1/barriers
- Räsänen, A. (2020). Papperslösa människor behöver hopp och sysselsättning. Retrieved 10/2021 from https://www.hdl.fi/sv/blog/papperslosa-manniskor-behover-hopp-och-sysselsattning/
- Sartorius N. (2006). The meanings of health and its promotion. Croatian medical journal, 47(4), 662–664.
- Savonius, A. (2017). Papperslösa vågar inte använda akut sjukvård - rädda för polis och avvisning. Retrieved 10/2021 from https://svenska.yle.fi/artikel/2017/05/23/papperslosa-vagar-inte-anvanda-akut-sjukvard-radda-polis-och-avvisning
- Semler, E. (2021). Finland’s North Karelia Project: Structural Barriers to Changing a Food Economy. American Journal of Public Health, 111(5), 785–786. https://doi-org.ezproxy.novia.fi/10.2105/AJPH.2021.306250
- Singu, S., Acharya, A., Challagundla, K., & Byrareddy, S. N. (2020). Impact of Social Determinants of Health on the Emerging COVID-19 Pandemic in the United States. Frontiers in public health, 8, 406. https://doi.org/10.3389/fpubh.2020.00406
- Tulane University. (2021). Education as a Social Determinant of Health. Retrieved 8/2021 from https://publichealth.tulane.edu/blog/social-determinant-of-health-education-is-crucial/
- Weida EB, Phojanakong P, Patel F, Chilton M.(2020). Financial health as a measurable social determinant of health. PLoS ONE 15(5): e0233359. https://doi.org/10.1371/journal.pone.0233359
- World Health Organization, WHO. (2012). Addressing the social determinants of health: The urban dimension and the role of local government. Retrieved 9/2021 from https://www.euro.who.int/__data/assets/pdf_file/0005/166136/UrbanDimensions.pdf
- World Health Organization, WHO. (2010). Equity, social determinants and public health programmes.Retrieved9/2021from http://apps.who.int/iris/bitstream/handle/10665/44289/9789241563970_eng.pdf;jsessionid=44B577717CC42D241BF715A58715DDCE?sequence=1
Studerandebloggen
Ansvarsfriskrivning: Författaren/författarna ansvarar för för fakta, möjlig utebliven information och innehållets korrekthet i bloggen. Texterna har genomgått en granskning, men de åsikter som uttrycks är författarens egna och återspeglar inte nödvändigtvis Yrkeshögskolan Novias ståndpunkter.
Disclaimer: The author(s) are responsible for the facts, any possible omissions, and the accuracy of the content in the blog.The texts have undergone a review, however, the opinions expressed are those of the author and do not necessarily reflect the views of Novia University of Applied Sciences.